Gluten causes a wide range of symptoms; that's a given. So, when a gluten-intolerant individual experiences a burning sensation after eating a meal, their first thought might be to blame gluten as the culprit.
But, can the reason be acid reflux, especially in the case of gluten-intolerant people? We have everything you want to know about gluten and acid reflux.
Gluten and Eating A Gluten-Free Diet
You have probably heard stories and myths about gluten, with it being a hot topic nowadays. But what, exactly, is gluten? Well, it's a group of proteins in abundance in wheat, barley, and rye.
Usually, proteins are vital for a healthy lifestyle and even survival and perform many fundamental functions. Hair, nails, and skin, for instance, require protein for proper formation. Proteins are an essential energy source in addition to bolstering the immune system.
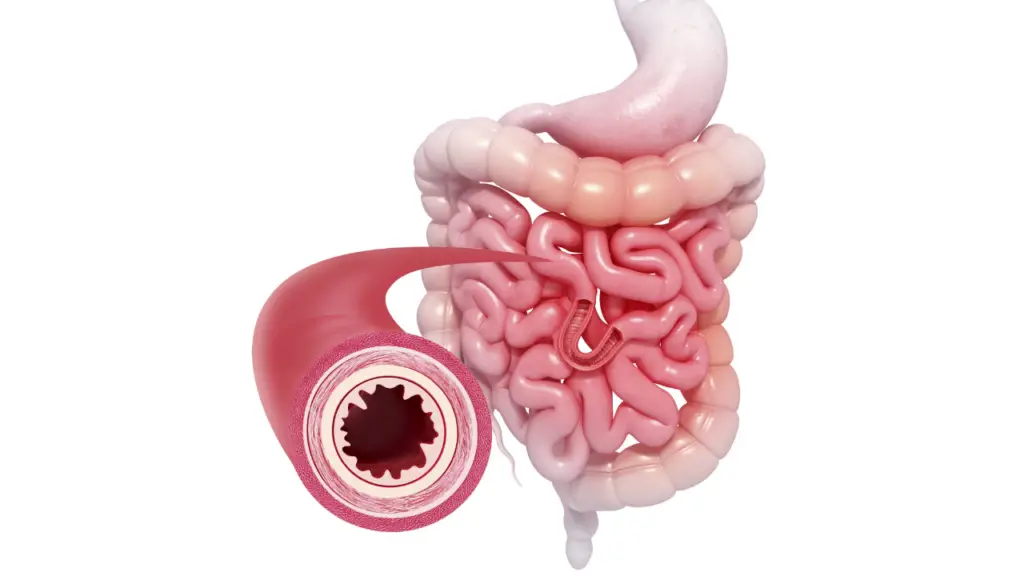
But gluten is dangerous and harmful for some people, and the same immune system bolstered by proteins starts to act against gluten. A person's body produces antibodies to get rid of gluten. But, in doing so, the antibodies also end up damaging the small intestine.
This condition is called celiac disease, an autoimmune disorder that nearly affects almost 2 million Americans and about 1 percent of the total global population.
When celiac individuals continuously eat gluten-containing foods, their immune system keeps getting triggered. Therefore, with every meal, their small intestine keeps getting damaged.
What Are The Symptoms?
The typical symptoms after a meal are bloating, diarrhea, and constipation, but patients have also complained about non-gastrointestinal symptoms. Our small intestine is responsible for absorbing nutrients. But when the small intestinal lining keeps getting damaged, it will lose its capability to absorb nutrients, eventually resulting in a deficiency of various nutrients.
This damage is the basis of most of the atypical symptoms, which vary from person to person. You'll be amazed to know that undiagnosed celiac disease can even cause issues such as dark circles under your eyes. Therefore, patients with celiac disease need to stay as far away from gluten, and its sources, as they possibly can.

If you're diagnosed with celiac disease, ask your dietitian for a gluten-free diet plan. Anything that contains gluten less than 20ppm is considered safe, and all such food items are collectively called “gluten-free” products.
Experts have yet to discover a treatment for celiac disease. The only way you can heal your small intestine and find relief from your symptoms is by going gluten-free. You can find processed gluten-free foods and altered versions of recipes of gluten-containing dishes. Although, it's always better to go for naturally gluten-free foods such as meat, dairy products, fruits, and vegetables.
Explaining Acid Reflux
Ever had the feeling your chest is on fire after having a meal containing citrus or something spicy? This condition of chest burning, bloating with a gassy stomach, and a bitter taste in the throat is known as acid reflux.
While some people call it heartburn or acid indigestion, it's normal to experience this every once in a while. But it's your body shouting to you about an underlying digestive problem if you experience any of these symptoms frequently or daily.
There's a muscle that forms a border between the esophagus and the stomach. It allows one-way traffic from the esophagus to the stomach. And, once the food has passed into the stomach for further digestion, this circular sphincter tightens and closes the passage.
When this muscle fails to contract or is too weak, the acid secreted by the stomach for digestion can enter the esophagus and damage its delicate lining, thus producing the effects of heartburn, and hence the name acid reflux.
Remember the iconic scene of The Lord Of The Rings where Gandalf screams “you shall not pass” to the fiery giant? Well, the lower esophageal sphincter acts as Gandalf to stop the burning acid from entering the esophagus.
If you're experiencing heartburn, your Gandalf is too weak to stop the acid. Acid reflux and consequential heartburn can be due to any habit, such as eating just before sleeping or because of certain food items, such as coffee, citrus fruits, or spicy foods.
What If The Symptoms Continue?
If you experience the symptoms of acid reflux more than twice a week, you're suffering from its chronic form, called gastroesophageal reflux disease or GERD. The symptoms are more severe and prolonged and even include dental erosion and asthma.
Since it's a chronic condition, it is likely caused by long-term issues either because of faulty anatomy or unhealthy habits. Hiatal hernia, for instance, is a condition that makes it difficult for the sphincter to tighten by reducing the pressure.
The hormone progesterone also triggers the symptoms of acid reflux by relaxing the lower esophageal sphincter. It's due to the excessive secretion of the hormone progesterone.
Gladly, the symptoms, like all other pregnancy-induced complications, are not lifelong and go away once the baby is born. Similarly, obesity, alcohol consumption, and smoking can lead to the onset of GERD.
Is Gluten to Blame for Acid Reflux?
Gluten is not harmful to everyone. Gluten-intolerant individuals will observe physical and mental symptoms, but they don't extend to healthy individuals. Gluten doesn't always cause severe complications.
So, the real question is whether gluten causes acid reflux in people with celiac disease and if there's a link between gluten and acid reflux, and even then, there's a lot of uncertainty.

Many researchers have proved by conducting experiments that gluten can cause heartburn in people who can't tolerate gluten. But many experts in the medical field and even individuals are adamant that their acid reflux isn't because of gluten intake. They don't suffer from other gastrointestinal symptoms, and even some atypical ones, but not the symptoms of acid reflux. So the answer to the question “does gluten cause acid reflux” is yes and no.
In some patients, gluten can cause heartburn, while in other people who have celiac disease, gluten does not trigger the symptoms of acid reflux. You can say the same about GERD. Considering the patient has tested negative for H pylori infection, a bacterial infection primarily responsible for the onset of GERD, there's a chance that they have their symptoms of GERD and peptic disease flared up because of gluten intake.
Is Gerd The Same As Acid Reflux?
Many researchers conducted studies published in the journal Clinical Gastroenterology and Hepatology. In March 2011 it proved that patients with undiagnosed celiac disease had a higher predisposition to GERD and acid reflux. It compared healthy people, meaning eating gluten can cause acid reflux in people with celiac disease.
There exists a link between gluten and acid reflux that is pronounced in some people and entirely masked in others but to consider it a rule of thumb that gluten does or doesn't cause acid reflux won't be an accurate assumption. It comes down to how you, yourself, react to gluten.

If eating gluten-based foods causes heartburn along with other gastrointestinal symptoms such as bloating, diarrhea, and constipation. Then there's a high chance you have both celiac disease and GERD. But if you're okay while eating bread or devouring pizzas and pasta, your body isn't sensitive to gluten. It is safe to say that you most likely don't have to worry about having celiac disease that might cause acid reflux.
Does Going Gluten-Free Help?
If we've established that gluten potentially causes acid reflux, it won't take much to believe that going gluten-free also helps with the symptoms. Generally, people with GERD who complain about frequent chest burning are treated with Proton Pump Inhibitors or PPIs and antacids.
These reduce the pH or acidity of the stomach, which eventually provides relief to the symptoms. But forcefully decreasing stomach acidity, especially for a prolonged period, can have other harmful effects. It'll be a trade-off and not a good one, in which you'll be avoiding the symptoms of GERD to suffer from arguably worse symptoms later on.

Undiagnosed celiac disease means you're prone to deficiency diseases already. Taking these medications makes you even more vulnerable to vitamin and mineral deficiencies. There's a high risk of developing osteoporosis, a condition that results in bone degeneration, and you can even end up losing your fertility.
Plus, there will still be the typical gastrointestinal symptoms of celiac disease you'll have to deal with. So, going gluten-free is the ideal way to deal with acid reflux if your body is intolerant to gluten.
Can Eating A Gluten-Free Diet Eliminate Gerd?
Several studies and experiments prove that a gluten-free diet can provide relief to chest and throat burning along with bloating, diarrhea, and constipation. There was an interesting study published in the Journal of Gastroenterology and Hepatology. 105 patients with celiac disease following a strictly gluten-free diet were involved, along with a control group consisting of 30 healthy people.
Both of these groups were treated with Proton Pump Inhibitors for eight weeks. After the 8th week, 86 percent of the celiac patients were relieved of their GERD symptoms. Alternatively, only 67 percent of the people of the control group found their symptoms resolved.
After six months, only 20 percent of the celiac patients experienced a recurrence of the symptoms. After which they were excluded from any future follow-up. Follow-ups were conducted after a year, a year, and a half, and two years. And, none of the remaining celiac patients showed a recurrence.

While in the control group, 30 percent of the non-celiac patients showed a recurrence after six months. And, the percentage kept rising with each follow-up. 80 percent of the celiac patients following a strict gluten-free diet showed no GERD symptoms after two years of being off the medication.
The non-celiac patients who ate foods containing gluten kept getting worse once they were taken off the medicines. And only 15 percent of them got rid of the painful symptoms of acid reflux and GERD.
What Were The Results Of The Study?
This study was quite detailed, but it was enough to prove that going gluten-free can help increase the effectiveness of medications for treating GERD and acid reflux. Therefore, keeping the patients protected from the manifestations of acid reflux.
A doctor asked patients to post their acid reflux experiences and the effects of going gluten-free on his website. The website has about 81 stories of people who found their cure in going gluten-free. Many even attempted this as a last resort after every medication failed, and the only regret they had was not going gluten-free earlier.

So if your acid reflux is acting up because of gluten intake, going gluten-free is an effective treatment. It will also help you with your gastrointestinal symptoms alongside. It will be a case of “no grain, no pain” for you. But if you don't frequently feel your chest and throat burn, especially after a meal, then gluten isn't causing your acid reflux.
Conclusion
In the end, your health is your own, and you're the one who needs to take charge of it. If you notice any symptoms relating to another condition such as acid reflux. Then it is best to consult a doctor immediately before the case turns worse. A healthy gluten-free lifestyle recommended by a professional may be the answer to all your problems.