Symptoms of gluten intolerance correlate with several other digestive conditions like Irritable Bowel Syndrome (IBS). The relation is similar to the extent that it's possible to misinterpret one for the other, and it's not uncommon to do so. After all, they're long-term conditions, and both wreak havoc on the intestines and cause digestive problems.
By this point, you might have a few questions like should you eat gluten-free with IBS considering many report betterment after switching to the diet despite having IBS and not gluten intolerance. Don't worry; this is the guide you need to answer all your queries.
Defining IBS
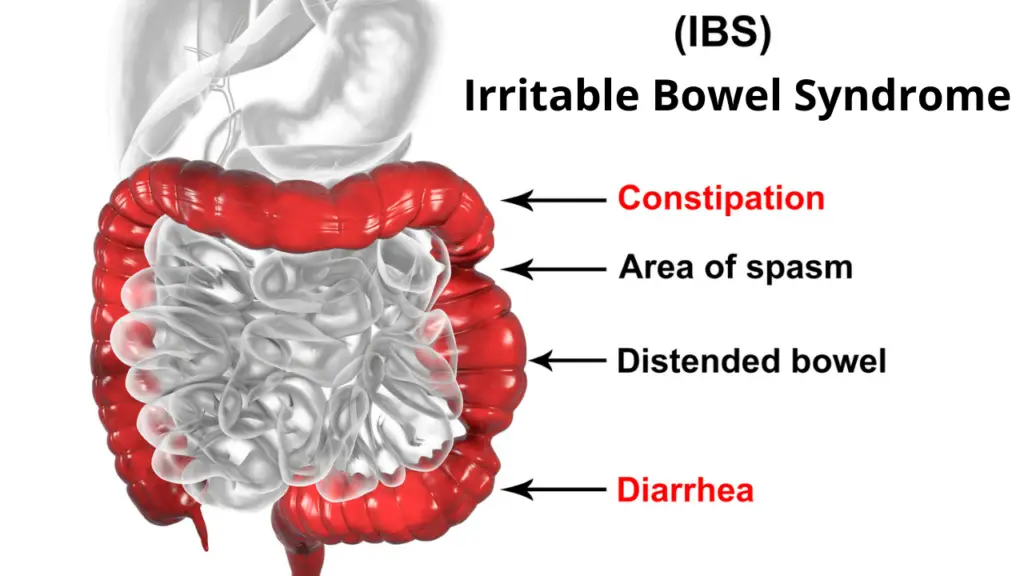
IBS or Irritable Bowel Syndrome, like other syndromes, is a collection of various intestinal symptoms. These symptoms include constipation, diarrhea, cramps, flatulence, and bloating.
With an affected large intestine, the patient may also complain about moderate to severe abdominal pain and nausea, in addition to unsuccessful attempts at emptying the bowels. Also called the spastic or irritable colon, your IBS can be of any one of these categories depending upon the symptoms, with each one being pretty self-explanatory; diarrhea-predominant or IBS-D, constipation-predominant or IBS-C, or mixed.
The muscles lining your intestine undergo rhythmical contraction for functional bowel movements. Thus, abnormalities in the contraction of these muscles lead to diarrhea or constipation. Prolonged contractions of greater strength cause diarrhea and flatulence, while weak contractions lead to constipation.
What Triggers IBS?

Perhaps the most common trigger for IBS is your daily diet intake. Certain food items increase the risks of flaring up the IBS symptoms. These are called dietary triggers. For instance, cereals and bread made from refined grains, alcohol, meals high in protein, and cheese have a knack to trigger your IBS-related constipation by aggravating the symptoms.
High fiber intake, fatty meals, and carbonated drinks can trigger diarrhea in an IBS-D patient. Dairy products containing lactose might have no harmful effects on many people, but the same food sources can kick start the diarrhea of a lactose-intolerant patient.
But your diet isn't the only element that can flare up IBS and its symptoms in your body. Several factors with a direct impact on your body can disrupt the movement of the intestines. For instance, a stress-induced lifestyle affects the brain, causing imbalance throughout the body's routine functionality.
Hormonal imbalance and drug usage can also disturb the physical wellbeing and can worsen IBS symptoms. To summarize, anything that throws your internal system out of balance, physical or psychological, can cause a harmful shift in your gut health, thus, leading to long-term IBS if not timely managed.
IBS and Gluten Intolerance- An Overview

Gluten intolerance is further divided into celiac disease and non-celiac sensitivity. The similarity between IBS and gluten intolerance are the digestive symptoms, i.e., abdominal pain, bloating, diarrhea, and constipation.
IBS is a set of symptoms, and almost all gluten intolerant individuals suffer from IBS, besides those who are asymptomatic. But not all IBS patients have gluten intolerance; they may be suffering because of other reasons.
It is known that celiac disease is an autoimmune disorder where the body produces antibodies against gliadin, the protein in gluten, and starts damaging the small intestines as a result. You could say celiac disease is a structural problem, i.e., there is actual damage happening inside your intestinal tract upon consuming gluten.
Non-celiac sensitivity is a reaction against gluten, which triggers digestive symptoms. But these gluten-sensitive individuals do not have an autoimmune disorder; it's just that their bodies can't absorb gluten as effectively, and they react to the gluten as well.
Lastly, IBS is a problem with the functionality of your bowel movement. The site of occurrence for IBS is primarily the large intestines. It's where undigested food creates problems and triggers digestive symptoms. IBS is more of a term for a combined group of symptoms rather than a condition due to a specific cause.
Identifying the Problems
Firstly, you'll need to identify the primary cause for the digestive symptoms you've been experiencing for some time. The symptoms need to be persistent for at least a few weeks. Otherwise, it could just be a temporary imbalance in your digestive system that goes away itself. To figure out what you need to be doing, you first need to recognize the symptoms as either celiac disease, gluten sensitivity, or IBS.
Diagnosing celiac disease is comparatively straightforward than the other two. You can consult a medical professional and opt for blood tests that determine whether your immune system is producing antibodies against gluten and consequently damaging the intestines. If the test comes out positive, a gluten-free lifestyle is your only choice. Meanwhile, if the test is negative, it could be one of the remaining two.
Gluten sensitivity and IBS trigger a similar set of digestive symptoms, including diarrhea, constipation, bloating, and abdominal pain. The difficulty is that neither of these two conditions can be diagnosed with medical tests yet.
You can self-diagnose to some extent or consult a doctor to correctly identify whether gluten is the culprit causing digestive problems in your body or something else. Eliminate gluten from your diet and gradually reintroduce it. If the symptoms decrease with elimination and come back once you start eating gluten again, gluten sensitivity is the answer.
On the other hand, IBS is not always caused by gluten, meaning gluten may be unconnected to your digestive symptoms. When the elimination and reintroduction process does not relieve your symptoms, it's a clear indication of IBS triggered by something other than gluten.
Low FODMAP Diet- A Solution to IBS?

FODMAP is an abbreviation for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, or short-chain carbohydrates. The body cannot digest these carbohydrates properly and push them out from the excretory system instead. FODMAPS undergo a process of fermentation in the gut while absorbing water.
The problem with high FODMAP foods is that since they're not readily absorbed in the intestines, excess quantity of these foods can lead to digestive imbalance. These poorly absorbed foods cater to digestive symptoms, including diarrhea, constipation, bloating, and abdominal pain, due to their indigestible nature.
A low FODMAP diet consists of foods with a decreased quantity of fermentable carbohydrates, which means the body can digest these without much trouble. Most, but not all, IBS patients show improvement once they shift to a low FODMAP diet. In a low FODMAP diet, your intestines mostly stay clean of fermented carbs piling in the colon.
It's safe to say that a low FODMAP diet may be the solution for IBS patients when nothing else works. In a low FODMAP diet, you'll avoid foods, such as dairy products, wheat-based products, beans and lentils, and high FODMAP fruits and vegetables.
As a result, the diet will contain poultry, specific cheeses, plant-based milk, low FODMAP grains, and low FODMAP fruits and vegetables. Around 86% of individuals with IBS who try out this diet report improvements in their condition.
Are Gluten-Free and Low FODMAP Diet Always the Same?
A gluten-free and low FODMAP diet differs in several ways, and you should never treat them similarly. A gluten-free diet is designed specifically for celiac or non-celiac sensitive patients. Meanwhile, a low FODMAP diet caters to IBS symptoms. Of course, anyone can follow either one of these diets or a combination of them.
Gluten intolerance necessitates a gluten-free diet, but incorporating low FODMAP in it is your choice. And IBS individuals may not find their symptoms relieved by following a gluten-free diet only. They'll have to shift towards a low FODMAP diet or add it to their existing gluten-free lifestyle.
Eating a Low FODMAP Diet – Will it Help your IBS?

As far as the diet plans go, a low FODMAP diet excludes wheat-based grains, which is what a gluten-free diet does as well. But a low FODMAP diet also eliminates other foods which are permittable when going gluten-free, e.g., all fruits and vegetables, non-gluten whole grains, any dairy product, and beans and lentils.
These foods are naturally gluten-free but contain a high ratio of fermentable carbs, making them unideal for a low FODMAP diet. Take another example. Amaranth, a pseudocereal, is naturally gluten-free, making amaranth flour gluten-free but not low FODMAP.
Low FODMAP foods, specifically processed foods, can contain hidden gluten. For instance, processed meat goes perfectly well in a low FODMAP diet, but many processed meat are susceptible to gluten.
That doesn't mean your life is over when it comes to following both diets. Low FODMAP natural produce is almost always gluten-free. You'll find millions of recipes on the internet that are low FODMAP, gluten-free, and sometimes even dairy-free!
But the higher possibility is that you won't have to restrict yourself to both diets for your symptoms- it's more likely either one or the other. Then again, there have been rare cases of patients who need to eliminate gluten and high FODMAP foods to reduce their symptoms. It isn't easy, but it's not impossible!
Gluten-Free for IBS- When Does it Work?

Gluten-free and low FODMAP diet have their differences, which is to say, a gluten-free diet doesn't always work for IBS patients. To recap, IBS has various causes, some of them being utterly unrelated to your diet intake. But studies prove that a gluten-free diet can relieve symptoms for those suffering from IBS too. So, what's the connection?
Your IBS symptoms can make a comeback when triggered by high FODMAP foods, mainly dairy, whole grains, beans and lentils, and some varieties of fruits and vegetables.
Now, the thing is that many people have problems with whole grains but have no problem ingesting the remaining high FODMAP food categories. Gluten-based grains are a source of gluten and fermented carbohydrates.
And, since a gluten-free diet eliminates gluten-based grains and their products, you're already excluding tons of troublemaking ingredients from your diet. Therefore, a gluten-free diet is beneficial for IBS patients considering gluten-based grains are a primary cause for their symptoms.
But that's not always the case, and if excluding gluten-based grains and products from your diet aren't improving your health, it's time to look towards other solutions like a low FODMAP diet.
Final Words

We have discussed numerous things that can help you decide if you should eat gluten-free if you have IBS. One is that gluten can cause issues in your digestive system. So eliminating gluten can most surely help reduce the pain you feel if you have IBS.
Always consult your physician first when deciding to change your diet. Diagnosing or delaying a medical appointment can put your health at stake when your digestive system is not responding accurately. You're only letting your body suffer when it shouldn't.
And a self-diagnosis between celiac diseases, non-celiac sensitivity, and IBS can often turn out incorrect. Follow the recommended diet strictly that your physician has given you. You deserve to feel the best you can and live a healthy life free from pain and suffering.





